The oil sands industry in Canada promises high wages and career opportunities, drawing workers from across the country. However, behind the economic appeal lies a much darker reality—the isolation of remote work camps and the ensuing addiction crisis. Separated from family, friends, and the comforts of home for weeks or even months at a time, many oil sands workers find themselves battling loneliness, depression, and substance abuse, often with devastating consequences.
The Isolating Reality of Work Camps
Oil sands work camps are typically located in remote areas, far from towns and cities. Workers live in communal facilities, often sharing cramped accommodations and following rigid schedules. Despite being surrounded by others, many feel profoundly isolated. The lack of personal freedom, the monotony of the daily routine, and the distance from loved ones contribute to a deep sense of loneliness.
For many workers, the isolation is compounded by the long shifts—12 or more hours a day for several weeks straight—followed by brief periods of leave. This “fly-in, fly-out” lifestyle can disrupt personal relationships and sever social ties, leaving workers feeling disconnected and emotionally adrift.
The Link Between Isolation and Substance Abuse
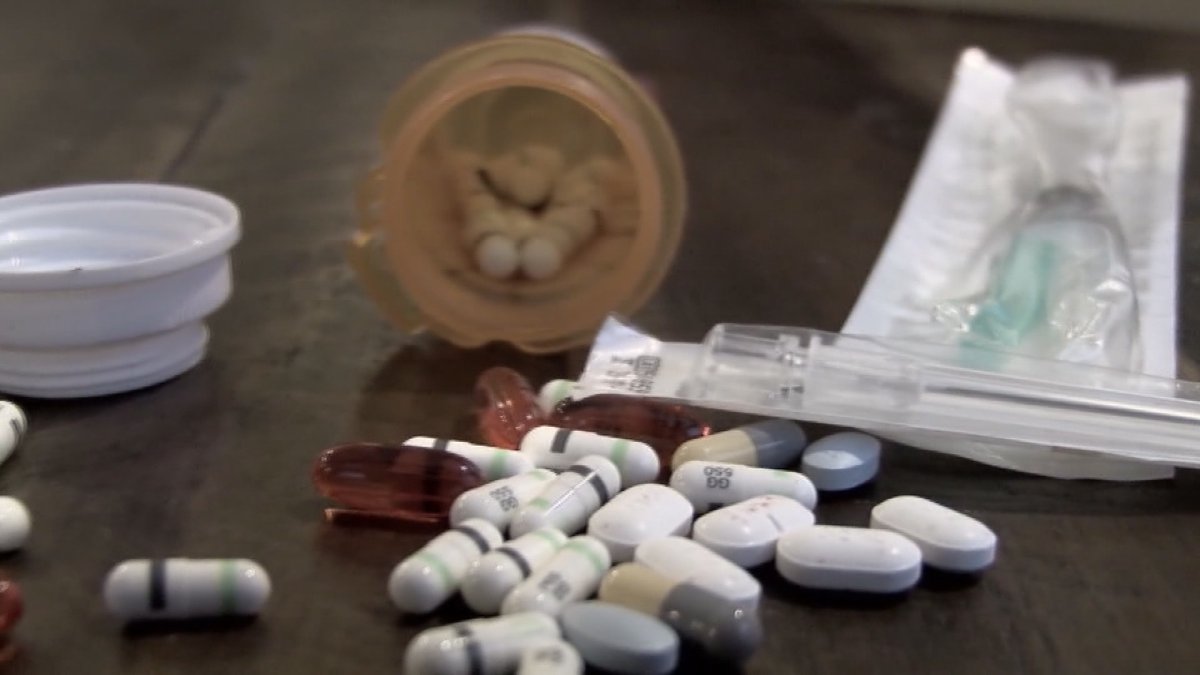
Isolation is a known risk factor for addiction, and oil sands workers are particularly vulnerable. Without access to healthy coping mechanisms or mental health resources, many turn to alcohol and drugs to numb their feelings of loneliness, boredom, and stress. Substance use can start as a way to “unwind” after a grueling shift but can quickly spiral into dependence.
Alcohol is often readily available in work camps, despite official policies prohibiting its excessive use. Some workers also use opioids to manage chronic pain from physically demanding labor or stimulants like cocaine and methamphetamine to combat fatigue. Over time, substance abuse becomes normalized, creating a camp culture where drug and alcohol use are pervasive and often go unnoticed or unaddressed.
Consequences for Workers and Communities
The consequences of isolation-driven addiction are severe. Workers struggling with substance abuse are at higher risk for accidents, which is particularly concerning in an industry involving heavy machinery and hazardous conditions. Addiction also affects mental health, leading to depression, anxiety, and an increased risk of suicide.
Beyond the camps, surrounding communities such as Fort McMurray face the ripple effects. There is a growing burden on healthcare systems, law enforcement, and social services to manage the fallout of addiction-related issues. Families back home also suffer, as addiction strains relationships and destabilizes households.
Steps Toward Solutions
Addressing the crisis of isolation and addiction in oil sands work camps requires systemic change. Companies must prioritize the mental well-being of their employees by offering accessible mental health services, confidential counseling, and substance abuse treatment programs. Creating more social and recreational opportunities within camps can help alleviate feelings of isolation.
Employers should also encourage a culture of openness, where seeking help is seen as a sign of strength, not weakness. Regular mental health check-ins and peer support programs can create a supportive environment where workers feel less alone.
Conclusion
The oil sands industry cannot ignore the dark side of isolation and addiction any longer. By recognizing the human cost behind the economic engine, and by investing in the mental health and well-being of workers, the industry can create safer, healthier work environments where individuals thrive rather than struggle in silence.